What doesn’t make us “tick”, are tick-borne diseases… they can be rewarding, straight-forward, text-book cases, but they can also throw you a curveball with a myriad of nasty complications.
In this post, you are going to find out:
- how pets get infected,
- which ticks can cause disease,
- the parasites that cause the illness,
- the two most common tick transmitted diseases we see in general practice,
- which symptoms to looks out for, and
- what you can do about it.

How do they get it?
Tick borne diseases are actually caused by tiny parasites that ticks can carry, rather than the ticks themselves. In order for a pet to get sick from a tick bite, a specific species of tick carrying a very specific parasite needs to bite and feed on your pet (the “host”) for 48 to 72 hours. Not all ticks carry the parasite, but if a “healthy” tick bites an infected pet, they will then become a carrier and can transmit the disease to another animal.

Babesiosis (tick bite fever, biliary, “bosluiskoors”)
In South Africa’s Southern Cape region, this is the most common and widely known tick borne disease. It can be contracted by both cats and dogs. In fact, it’s common among our coastal feline population, but is hardly ever seen in cats outside our coastal areas. Cats from inland and especially those with compromised immune systems are particularly at risk of contracting Babesiosis.
The tick
For dogs, the culprit which causes Babesiosis is the yellow dog tick (Haemaphysalis leachi). In cats, the exact tick or ticks causing feline biliary have not yet been established for certain. Seeing that it only affects cats on our coastal regions, we can deduct that it must be ticks limited to this geographical area.

The yellow dog tick (Haemaphysalis leachi)
Image replicated from "A guide to animal diseases in South Africa - Cats and Dogs" by Pamela Oberem
The parasite
These ticks carry dangerous parasites. In dogs, this is a microscopic, single-celled protozoan called Babesia canis. In cats, two tiny protozoa parasites cause biliary – Babesia felis and Mycoplasma.
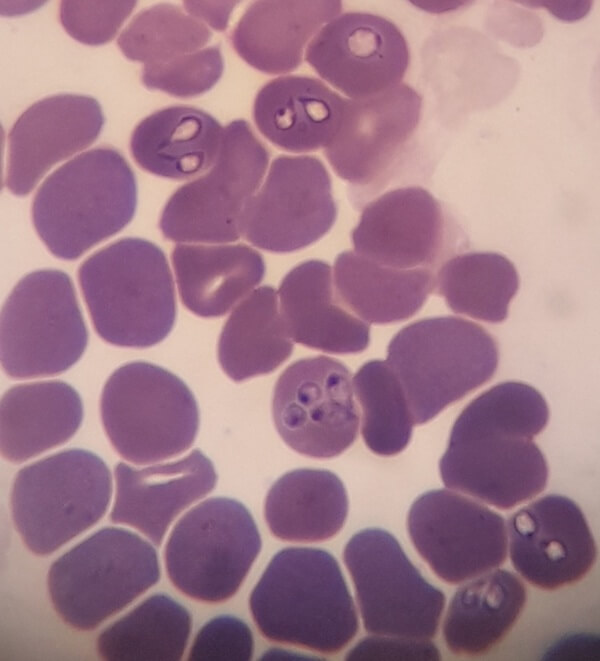
Babesia canis parasites in a dog as seen under the microscope
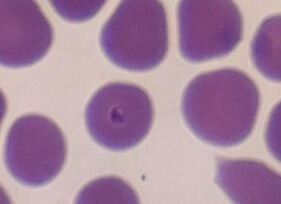
Babesia felis parasite
Cats can develop mild disease and remain carriers, with flare-ups of illness during times of stress.
In its initial stage, the parasite enters the host’s bloodstream and infects the red blood cells, which carry oxygen from the lungs to the rest of the body. Here they start to multiply and wreak havoc. To diagnose this disease, your vet will make a blood smear and look for these parasites under the microscope.
Symptoms of the disease
Anorexia
The very first sign that you might notice of a biliary infection is that your usually very greedy pooch refuses his or her food. This is also true for cats – a species that is notorious for hiding signs of illness.
Fever
The multiplication of the parasite in the red blood cells causes a fever in the body as it tries to fight off infection. This is a necessary infection control mechanism, but it can cause problems if left unchecked. A very low body temperature, on the other hand, generally indicates a poorer prognosis as it means that the body is unable to cope anymore.

Fever in a dog. The normal body temperature for dogs and cats is around 37.5०C and 38.5०C
Pale gums
The infected red blood cells die and the iron-rich haemoglobin inside the cell is released. The loss of red blood cells eventually causes anaemia, which results in visibly pale gums.

Pale gums with a slight yellow-tinge in a dog with biliary.
Jaundice
The broken down red blood cells need to be processed by the liver, and this increases the liver’s workload. If the liver cannot keep up, free haemoglobin accumulates in the blood causing jaundice (icterus) – and your pet’s gums will turn yellow.

A very jaundiced cat
Auto-immune haemolytic anaemia
This awful complication happens when the infected, dying red blood cells trigger a severe immune reaction and your ill pet’s own immune system starts attacking itself, killing off more red blood cells. The anaemia gets even worse.
Cerebral babesiosis
Shockingly, the parasites can enter and accumulate in the micro brain blood vessels, causing damage to these tiny blood vessels, as well as severe inflammation and cell death in the brain. It can become very difficult to treat and cause all sorts of neurological problems. The neurological signs one might see include loss of balance, incoordination, nausea, altered consciousness and even seizures. Cerebral babesiosis is often fatal. Fortunately, this is a very rare complication.
The treatment
Dogs
Uncomplicated biliary cases need nothing more than an effective anti-protozoal treatment, some rest, and TLC at home. Diminazene (Berenil) and Imidocarb (Forray) are the most commonly used treatments. Keep in mind that the safety margins of these anti-protozoal treatments are extremely narrow and they can be toxic if given at the incorrect dose. Self medicating your pet at home is therefore never recommended.
Fun fact: the very first anti-protozoal treatment for babesia, developed in the early 1900’s, was Trypan Blue. This azo dye coloured dead tissue and cells blue, turning pets treated with this relatively safe drug an eerie blue-green hue!
Complicated biliary cases will need hospitalisation with more extensive treatment depending on the circumstances. Most will need a life-saving blood transfusion if the anaemia is too advanced. Auto-immune haemolytic anaemia patients will need immunosuppressors like steroid treatment. Cerebral babesia cases with seizures will need anti-epileptic treatment and careful monitoring. Your pet might have to be hospitalised on a drip for several days with liver support remedies.

Puppy receiving a blood transfusion
Cats
The anti-malarial drug primaquine phosphate is the drug of choice for treating biliary in cats. This treatment involves a course of tablets: the first three doses are three days apart, followed by single, weekly doses. This treatment doesn’t actually kill off the parasites; hence our local cats seem to live happily with a few parasites and no apparent effect on their health. Your vet will make an informed decision on whether to start treatment for biliary, or to look for other causes that could be making your cat unwell. The preferred treatment for mycoplasma is a 3 weeks course of an antibiotic called doxycycline.
Ehrlichiosis (“bosluisbytkoors”)
Ehrlichia is a less commonly noticed tick-borne disease that we see at our practice. It only affects dogs.
The tick
The accused tick is the brown dog tick, aka the kennel tick (Rhipicephalus sanguineus).

The kennel tick (Rhipicephalus sanguineus)
Image replicated from "A guide to animal diseases in South Africa - Cats and Dogs" by Pamela Oberem
The parasite
The parasite causing the illness is a rickettsia called Ehrlichia canis. This little parasite enters its host – your dog – through a brown dog tick feeding off its host’s blood. It enters the host’s bloodstream and infects the white blood cells, causing inflammation of the blood vessels and platelet consumption (the blood cells that play a major role in blood clotting), causing a decrease in platelet count.
Your vet will do a blood smear and use a microscope to look for signs of the parasite inside your pet’s white blood cells. Even if no parasite is spotted, a low platelet count and an increase in certain types of white blood cells are good reasons to suspect ehrlichia, and your vet will discuss sending a blood sample to the laboratory for confirmatory testing.
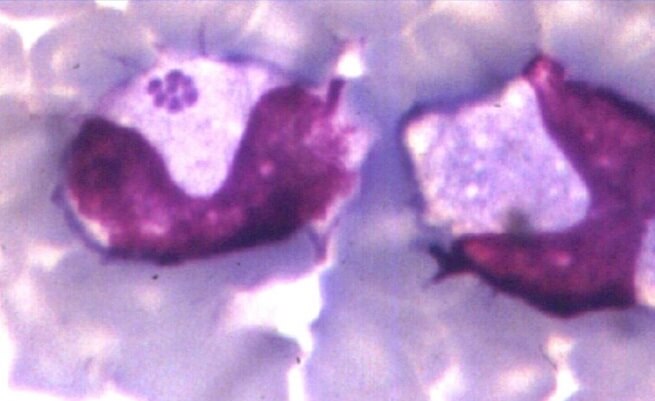
Ehrlichia morula in the white blood cell (monocyte) of a dog as seen under the microscope.
Photo credit Prof. Fred Reyers
The disease
Sadly, ehrlichiosis can progress from a short-term to a long-term disease.
Initially you may notice:
- loss of appetite,
- depression,
- fever,
- loss of stamina,
- stiffness and reluctance to walk,
- swelling of the legs,
- widespread swelling of the lymph nodes or glands,
- a big spleen – which you might see as abdominal distension or abdominal pain,
- pale gums,
- a tendency to bleed spontaneously, and areas of bruising on the skin (petechiae) due to a decrease in the number of platelets,
- bleeding from the nose, blood in urine or stool, etc.,
- coughing or difficulty breathing.
More chronic cases can present in many forms with an array of organ involvement. Possible scenarios, just to mention a few, include
- vomiting,
- chronic diarrhoea,
- an enlarged spleen,
- widespread bleeding (eg. nose bleeds),
- kidney failure,
- inflammation of the lungs, eyes, or brain and spinal cord (If the brain and spinal cord are affected, lack of coordination, depression, partial paralysis and increased sensitivity to touch can be seen),
- severe weight loss is common with chronic ehrlichiosis.
The treatment
Your vet will prescribe a long course of an antibiotic called doxycycline.
More complicated or chronic cases will need more aggressive treatment depending on the case. This might involve a blood transfusion or drip fluids, and supportive care.
Ticking off
I think we’ve pretty much “ticked” off all the noteworthy points surrounding tick-borne diseases. You can now appreciate why these diseases are best avoided. Unfortunately, not all patients survive these preventable, curable infections.
Happily, thanks to recent developments in tick control products, tick transmitted diseases in dogs and cats are now much less prevalent. Keeping your pet free of parasite-infected crawlies can be as simple as feeding him or her a tasty, medicated pill. Feel free to drop in anytime and enquire about our tick control products on offer – these are over the counter medications and you won’t need a prescription or an appointment.




